The Role of Blood Thinners in Preventing Heart Disease

Table of Contents
- Understanding Heart Disease Risk
- Types of Blood Thinners
- Mechanism of Action
- Benefits of Blood Thinners
- Considerations for Patients
Understanding Heart Disease Risk
Heart disease is a leading cause of death worldwide, and understanding your individual risk factors is crucial in preventing it. Several factors can contribute to an increased risk of developing heart disease, and knowing them can help you take proactive steps towards a healthier heart. Here are some key factors that play a role in determining your heart disease risk:
- Family history: If there is a history of heart disease in your immediate family, such as parents or siblings, your risk may be higher.
- Age: As we age, the risk of heart disease tends to increase. Men over the age of 45 and women over the age of 55 are at a higher risk.
- Smoking: Smoking is a significant risk factor, as it damages the blood vessels and increases the likelihood of atherosclerosis, a condition in which the arteries harden and narrow.
- High blood pressure: Hypertension, or high blood pressure, forces the heart to work harder, increasing the strain on the arteries and leading to heart disease.
- High cholesterol: Elevated levels of LDL (bad) cholesterol can contribute to the buildup of plaque in the arteries, increasing the risk of heart disease.
- Diabetes: People with diabetes are at a higher risk of heart disease due to the damaging effects of high blood sugar on the arteries.
- Physical inactivity: Living a sedentary lifestyle can contribute to obesity, high blood pressure, and other risk factors for heart disease.
- Obesity: Being overweight puts additional strain on the heart and increases the likelihood of developing other risk factors for heart disease.
While these risk factors can increase your chances of developing heart disease, they are not definitive guarantees. By adopting a heart-healthy lifestyle, you can lower your risk and potentially prevent heart disease. Regular physical activity, a balanced diet that is low in saturated fats and rich in fruits, vegetables, and whole grains, maintaining a healthy weight, avoiding smoking, and managing stress levels are all essential components of a heart-healthy lifestyle.
In some cases, individuals with a high risk of heart disease may be prescribed blood thinners by their healthcare providers. These medications, also known as anticoagulants, can help prevent blood clots from forming in the arteries, reducing the risk of a heart attack or stroke. However, blood thinners should only be used under the guidance of a medical professional, as they can have side effects and require careful monitoring.
It is important to remember that heart disease is a complex condition, and each individual’s risk factors and needs may vary. Regular medical check-ups, discussions with healthcare providers, and following a personalized prevention plan are essential in managing heart disease risk. By understanding your risk factors and taking proactive steps towards a heart-healthy lifestyle, you can improve your overall cardiovascular health and well-being.
Types of Blood Thinners
Blood thinners, also known as anticoagulant medications, are commonly prescribed drugs that help prevent heart disease and other serious medical conditions. They work by reducing the blood’s ability to clot, thereby preventing the formation of blood clots that could lead to heart attacks or strokes. There are several different types of blood thinners available, each with its own unique characteristics and risks. Let’s explore some of the most commonly used blood thinners:
- Warfarin (Coumadin): Warfarin has been used for decades and is one of the most commonly prescribed blood thinners. It works by interfering with the body’s ability to use vitamin K to produce clotting factors. Regular monitoring of the international normalized ratio (INR) is necessary to ensure the medication’s effectiveness and safety.
- Direct Oral Anticoagulants (DOACs): DOACs, such as apixaban, dabigatran, edoxaban, and rivaroxaban, are newer blood thinners that have gained popularity due to their convenience. Unlike warfarin, DOACs do not require regular INR monitoring. However, their effectiveness may vary depending on factors like kidney function.
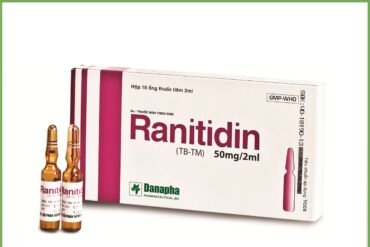
- Heparin: Heparin is available in two forms: unfractionated heparin (UFH) and low molecular weight heparin (LMWH). UFH is often administered through an intravenous (IV) line in a hospital setting, while LMWH is given as a subcutaneous injection at home. Both UFH and LMWH are rapidly acting blood thinners used for short-term treatment.
- Aspirin: While not as potent as other blood thinners, aspirin is commonly used as a preventive measure for heart disease. It inhibits the production of chemicals called prostaglandins that play a role in blood clotting.
It’s crucial to note that each blood thinner comes with its own risks and potential side effects. Some common risks associated with blood thinners include increased bleeding, particularly in cases of trauma or surgery. Patients taking blood thinners should regularly consult with their healthcare provider to monitor their dosage and ensure any potential drug interactions are considered. Additionally, lifestyle modifications, such as maintaining a healthy diet and exercise routine, can complement the benefits of blood thinners in preventing heart disease.
Mechanism of Action
When it comes to preventing heart disease, blood thinners play a crucial role. These medications work by altering the blood’s ability to clot, which helps in reducing the risk of blood clots that can lead to heart attacks and strokes. Blood thinners primarily act through one of the following mechanisms:
- Antiplatelet effect: Some blood thinners, such as aspirin, exert their effects by preventing platelets from sticking together. Platelets are small cell fragments in the blood that form the initial clotting plug at the site of injury. By inhibiting platelet aggregation, antiplatelet medications decrease the likelihood of clot formation in arteries.
- Anticoagulant effect: Other blood thinners, like warfarin or heparin, have anticoagulant properties. These drugs work by interfering with various steps of the blood clotting process. Anticoagulants slow down the production of clotting factors or inhibit specific proteins responsible for clot formation, reducing the overall blood clotting ability.
- Thrombolytic effect: Thrombolytic agents, such as tissue plasminogen activator (tPA), work differently than other blood thinners. Instead of preventing clotting, they actively break down existing blood clots. These medications are primarily used during acute events, such as heart attacks, to quickly dissolve the clot and restore blood flow.
Blood thinners are prescribed based on an individual’s risk factors and overall health. It’s important to note that these medications are not suitable for everyone and can have side effects. Regular monitoring, dose adjustments, and close communication with a healthcare provider are necessary when using blood thinners.
In conclusion, blood thinners have the ability to prevent heart disease by inhibiting platelet aggregation, interfering with the clotting process, or actively dissolving blood clots. The choice of blood thinner and its administration depends on several factors, including the individual’s medical history and condition. It is advisable to always consult with a healthcare professional to determine the most suitable blood thinner and its appropriate usage to minimize the risk of heart disease effectively.
Benefits of Blood Thinners
Blood thinners, also known as anticoagulants, play a crucial role in the prevention and management of heart disease. These medications are designed to inhibit the formation of blood clots, which can reduce the risk of heart attack, stroke, and other cardiovascular complications. Let’s explore some of the key benefits of using blood thinners:
- Preventing blood clots: One of the primary functions of blood thinners is to prevent the formation of blood clots. These medications help to keep the blood flowing smoothly through the arteries and veins, reducing the risk of blockages that can lead to heart attack or stroke.
- Reducing the risk of stroke: Blood clots can block the blood vessels that supply oxygen to the brain, causing a stroke. By keeping the blood thin, anticoagulants can significantly lower the chances of a stroke occurring.
- Managing existing heart conditions: Blood thinners are also prescribed to individuals with certain heart conditions, such as atrial fibrillation (irregular heart rhythm) or artificial heart valves. These medications prevent the formation of blood clots in these high-risk situations.
- Preventing deep vein thrombosis (DVT): Deep vein thrombosis occurs when a blood clot forms in the deep veins, usually in the legs. Blood thinners help to prevent DVT by inhibiting the clotting process, reducing the risk of a potentially life-threatening condition.
- Stabilizing angina: Angina is chest pain or discomfort caused by reduced blood flow to the heart. Blood thinners can help stabilize angina by preventing the formation of blood clots, improving blood flow, and reducing the frequency and severity of chest pain episodes.
It is important to note that while blood thinners offer numerous benefits, they also come with potential risks. These medications can increase the risk of bleeding, so individuals taking blood thinners should be cautious and follow their healthcare provider’s guidance regarding dosage and regular monitoring. Additionally, certain medications and foods may interact with blood thinners, so it is crucial to inform your doctor about all other drugs and dietary habits.
In conclusion, blood thinners play a vital role in preventing heart disease and managing various cardiovascular conditions. By preventing blood clots, reducing the risk of strokes, and stabilizing angina, these medications have proven to be highly effective. However, it is essential to take blood thinners under medical supervision to ensure proper dosage and minimize potential risks.
Considerations for Patients
When it comes to preventing heart disease, blood thinners play a crucial role. These medications help prevent blood clots from forming and reduce the risk of strokes or heart attacks. If you have been prescribed blood thinners or are considering them as a preventive measure, there are several important considerations to keep in mind:
- Consultation with a healthcare professional: It is crucial to consult with a healthcare professional, such as a cardiologist or primary care physician, before starting any blood thinners. They will assess your medical history, current health status, and assess the benefits versus the risks of blood thinners.
- Understanding the medication: Blood thinners are not all the same. There are different types available, and each works in a slightly different way. It is essential to understand the specific medication prescribed to you, including proper dosage and any potential side effects.
- Regular monitoring: Blood thinners require regular monitoring to ensure they are working effectively and that the dosage is appropriate. This may involve regular blood tests, such as the International Normalized Ratio (INR) test, to measure the clotting time of your blood.
- Lifestyle adjustments: While taking blood thinners, certain lifestyle adjustments are necessary. Inform your healthcare professional if you plan to make any dietary changes, start new medications, or engage in activities that may increase the risk of bleeding, such as contact sports.
- Medication interactions: It is essential to inform your healthcare professional about all medications you are taking, including over-the-counter drugs, supplements, or herbal remedies. Some medications, when combined with blood thinners, can increase the risk of bleeding or interfere with the medication’s effectiveness.
- Emergency preparedness: In case of an emergency or surgery, it is crucial to inform medical personnel that you are on blood thinners. They may need to take special precautions to prevent excessive bleeding or interact with the medication appropriately.
Remember, blood thinners are powerful medications that require careful consideration, proper education, and close monitoring when used for the prevention of heart disease. Always consult with a healthcare professional to determine if blood thinners are the right choice for you and to ensure a well-informed and safe management of your heart health.