Common Symptoms of Microscopic Polyangiitis
Table of Contents
- Persistent fatigue and weakness
- Recurrent sinus infections
- Skin rash and ulcers
- Joint pain and swelling
- Renal (kidney) involvement
Persistent fatigue and weakness
Persistent fatigue and weakness are common symptoms experienced by individuals with Microscopic Polyangiitis (MPA). This rare autoimmune disease primarily affects small blood vessels, leading to inflammation and damage in various organs, including the kidneys, lungs, and skin. Fatigue and weakness can significantly impact the quality of life for those living with MPA. Understanding and managing these symptoms is crucial for improving overall well-being.
Here are some important points to consider about persistent fatigue and weakness in MPA:
- Chronic nature: Fatigue and weakness in MPA tend to persist over time and may not improve with rest or sleep. This constant feeling of exhaustion can result in reduced stamina and an inability to perform daily activities.
- Contributing factors: Several factors can contribute to fatigue and weakness in MPA. Anemia, a condition in which there is a shortage of healthy red blood cells, is common among MPA patients and can lead to reduced oxygen delivery to the body’s tissues and organs, causing fatigue. Additionally, the immune system’s chronic activation in MPA can also contribute to ongoing lethargy and weakness.
- Impact on mental health: Persistent fatigue and weakness can have a significant impact on mental health, leading to feelings of frustration, depression, and reduced motivation. It is essential for individuals with MPA to seek support from mental health professionals to address these challenges and maintain overall well-being.
- Managing fatigue and weakness: While there is no specific cure for MPA-related fatigue and weakness, several strategies can help manage these symptoms. Regular exercise, tailored to individual capabilities, can improve energy levels and overall strength. It is important, however, to engage in activities that do not overexert the body. Nutritious, well-balanced meals and adequate hydration are also crucial in maintaining optimal energy levels.
- Seeking medical advice: If persistent fatigue and weakness are interfering with daily life, it is vital to consult with a healthcare professional. In some cases, additional medications, such as erythropoietin-stimulating agents or other treatments targeting anemia, may be prescribed to help alleviate these symptoms.
By understanding persistent fatigue and weakness in the context of Microscopic Polyangiitis, individuals with MPA can actively address these symptoms and improve their quality of life. Sharing concerns with healthcare providers, utilizing support services, and adopting strategies to manage fatigue can lead to better overall well-being.
Recurrent Sinus Infections
Recurrent sinus infections, also known as chronic sinusitis, are a common condition that affects many individuals worldwide. This condition occurs when the sinuses, which are hollow spaces within the bones of the face, become inflamed and infected. While acute sinusitis typically resolves within a few weeks, recurrent sinus infections persist and can significantly impact one’s quality of life.
Here are some common symptoms associated with recurrent sinus infections:
- Persistent Nasal Congestion: One of the hallmark symptoms of chronic sinusitis is the ongoing feeling of nasal blockage or congestion. This can hinder proper airflow and may lead to difficulty breathing.
- Facial Pain and Pressure: Individuals with recurrent sinus infections often experience pain and pressure in the face, particularly around the nose, forehead, and cheeks. This discomfort can vary in intensity and may worsen when bending forward or lying down.
- Nasal Discharge and Postnasal Drip: Thick, discolored nasal discharge or mucus draining down the back of the throat (postnasal drip) is a common symptom. This may lead to a persistent cough, throat irritation, and a noticeable unpleasant taste.
- Reduced Sense of Smell and Taste: Chronic sinusitis can affect the olfactory system, resulting in a diminished ability to smell and, subsequently, taste.
- Elevated Fatigue: Dealing with recurrent sinus infections can be tiring both physically and mentally. The ongoing inflammation and discomfort may leave individuals feeling fatigued and lacking energy.
- Bad Breath: Bacteria and mucus accumulation can cause persistent bad breath, known as halitosis, in individuals with chronic sinusitis.
- Headaches: Frequent headaches, especially in the forehead area, are often reported by individuals with recurring sinus infections.
If you experience any combination of these symptoms, it is important to consult with a healthcare professional for an accurate diagnosis and appropriate treatment. Treatment may include antibiotics to address bacterial infections, nasal corticosteroids to reduce inflammation, saline nasal irrigation, or in some cases, surgery to clear blocked sinuses.
Understanding the symptoms associated with recurrent sinus infections can help individuals seek timely medical intervention and alleviate the discomfort associated with this condition.
Skin Rash and Ulcers
Skin rash and ulcers are common symptoms experienced by individuals with microscopic polyangiitis. This condition is a systemic vasculitis that primarily affects small blood vessels. When these blood vessels become inflamed, it can lead to various complications, including skin manifestations such as rashes and ulcers.
The skin rash seen in microscopic polyangiitis can present in different forms. It may appear as small red or purple dots, called petechiae, on the skin. These dots may be flat or slightly raised and are often clustered together. Another type of rash seen is purpura, which are larger bruises-like patches on the skin. These rashes are typically painless but can be alarming due to their appearance.
In addition to rashes, individuals with microscopic polyangiitis may also develop skin ulcers. Ulcers are open sores that occur when the skin breaks down or dies. These ulcers can be painful and may be accompanied by symptoms such as tenderness, redness, and swelling in the affected area. Ulcers commonly occur on the lower legs and feet, but they can also develop in other areas of the body.
It is important to understand that the presence of skin rash and ulcers in microscopic polyangiitis is often a result of the underlying vasculitis affecting the blood vessels. The inflammation compromises the blood flow and can lead to skin-related complications. If left untreated, these conditions can worsen and potentially cause serious infections.
If you or someone you know experience skin rash or ulcers along with other symptoms such as fatigue, joint pain, fever, or organ dysfunction, it is crucial to seek medical attention. A healthcare professional can conduct a thorough evaluation, perform diagnostic tests, and provide appropriate treatment.
Treatment for skin rash and ulcers in microscopic polyangiitis typically involves managing the underlying vasculitis. This may include the use of immunosuppressive medications to reduce inflammation and control the progression of the disease. Alongside medical treatment, lifestyle modifications and self-care measures can also help in improving symptoms and promoting overall well-being.
- Keep the affected areas clean and dry.
- Avoid scratching or picking at the rash or ulcers.
- Wear loose-fitting clothing to prevent friction and irritation.
- Apply moist dressings or prescribed topical medications to promote healing.
- Follow a balanced diet and stay hydrated to support the healing process.
- Engage in gentle exercises to improve blood circulation and prevent stiffness.
- Take prescribed medications as directed by your healthcare provider.
- Attend regular follow-up appointments to monitor your condition.
Remember, timely diagnosis and appropriate management of microscopic polyangiitis can help alleviate symptoms and prevent further complications. Consulting a healthcare professional is essential for an accurate diagnosis and tailored treatment plan.
Joint Pain and Swelling
Joint pain and swelling are common symptoms experienced by individuals with microscopic polyangiitis. This rare autoimmune disease affects small blood vessels in various organs, including the joints, leading to inflammation and damage. Joint involvement is often seen in the initial stages of the condition and can be quite debilitating. Understanding and managing joint pain and swelling is crucial for individuals living with microscopic polyangiitis.
Here are some key points to know about joint symptoms associated with microscopic polyangiitis:
- Pain and Stiffness: Joint pain is a hallmark of microscopic polyangiitis. It commonly affects large joints like the knees, hips, and shoulders. The pain may be severe and can limit mobility. Stiffness in the affected joints is also observed, especially after periods of inactivity.
- Swelling and Warmth: Swelling around the affected joints is another common feature. The joints may appear red and warm to the touch due to inflammation. This swelling can restrict joint movement and cause discomfort.
- Systemic Symptoms: Joint pain and swelling in microscopic polyangiitis often accompany other systemic symptoms such as fever, fatigue, weight loss, and muscle aches. These symptoms indicate the widespread nature of the disease.
- Flares and Remissions: Joint symptoms may come and go, with periods of flare-ups followed by remissions. This pattern can vary greatly among individuals, and the duration and intensity of flare-ups can differ each time.
- Management and Treatment: To alleviate joint pain and swelling, various treatment approaches are used. Doctors may prescribe nonsteroidal anti-inflammatory drugs (NSAIDs) to manage pain and reduce inflammation. Immunosuppressive medications like corticosteroids or disease-modifying antirheumatic drugs (DMARDs) may be recommended to control the underlying autoimmune response.
If you experience joint pain and swelling along with other worrisome symptoms, it is essential to seek medical attention promptly. A healthcare professional can evaluate your condition, conduct necessary tests, and devise an appropriate treatment plan to alleviate your symptoms and manage microscopic polyangiitis effectively.
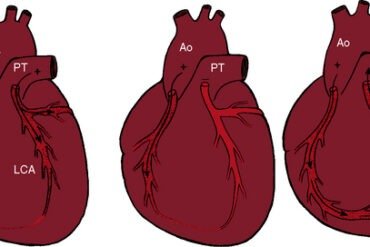
Renal (Kidney) Involvement
Microscopic Polyangiitis (MPA) is a rare autoimmune disease characterized by inflammation of small blood vessels, primarily affecting the kidneys, lungs, and other organs. Renal involvement is a significant hallmark of MPA and can lead to severe kidney damage if left untreated.
Here are the common symptoms of renal involvement in Microscopic Polyangiitis:
- Hematuria: One of the primary symptoms of renal involvement is the presence of blood in the urine. It can present as pink, brown, or red-colored urine.
- Proteinuria: Another common symptom is the presence of excess protein in the urine. This can lead to frothy urine, swelling in the hands, legs, and face (edema), and unexplained weight gain.
- Decreased Urine Output: Renal involvement in MPA can impair kidney function, leading to a decrease in urine production. This may result in frequent urination, intense thirst, and fluid retention.
- Hypertension: High blood pressure is a frequent occurrence in individuals with renal involvement. It can be a consequence of kidney damage and reduced urine output.
- Renal Insufficiency: As the disease progresses, the kidneys may lose their ability to effectively filter waste and toxins from the blood. Consequently, renal insufficiency can lead to symptoms like fatigue, nausea, vomiting, and a general sense of unwellness.
- Renal Failure: In severe cases, untreated renal involvement can progress to kidney failure, where the kidneys are unable to maintain the body’s normal internal environment. This may require dialysis or kidney transplantation to sustain life.
If you experience any of these symptoms or suspect renal involvement, it is crucial to seek immediate medical attention. Early diagnosis and treatment can help manage the disease, prevent irreversible kidney damage, and improve long-term outcomes.