Recognizing the Symptoms of Neonatal Intraventricular Hemorrhage

Table of Contents
- Overview of Neonatal Intraventricular Hemorrhage
- Common Risk Factors and Causes
- Early Signs and Symptoms to Look Out For
- The Importance of Prompt Diagnosis and Treatment
- Long
- Term Effects and Complications
Overview of Neonatal Intraventricular Hemorrhage
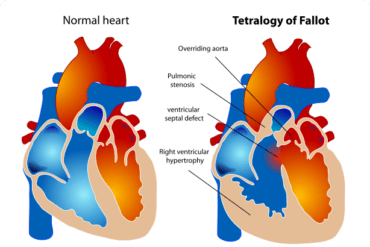
Neonatal intraventricular hemorrhage (IVH) refers to bleeding in the brain’s ventricular system, typically occurring in premature infants. This condition is a major concern as it can lead to significant morbidity and mortality in newborns. IVH is primarily categorized into four grades based on the severity of bleeding, with grade 1 being the mildest and grade 4 being the most severe.
Here is a brief overview of each grade:
- Grade 1: Minimal bleeding occurs within the germinal matrix, an area of the brain where new brain cells develop. This grade usually resolves without major consequences.
- Grade 2: Bleeding extends into the ventricles but does not cause dilation. Most infants with grade 2 IVH have a good prognosis, but they may experience developmental delays.
- Grade 3: Ventricular dilation accompanies bleeding, leading to increased pressure within the brain. Infants with grade 3 IVH may develop hydrocephalus, a condition characterized by excessive accumulation of cerebrospinal fluid.
- Grade 4: Severe bleeding occurs within the ventricles, resulting in significant ventricular dilation. Infants with grade 4 IVH often experience long-term neurological complications.
The symptoms of neonatal IVH can vary depending on the grade and extent of the bleeding. Common signs include:
- Changes in heart rate, blood pressure, or breathing patterns
- Seizures or abnormal body movements
- Pale or bluish skin color
- Weakness or lack of movement in limbs
- Difficulty feeding or swallowing
Early detection and management of neonatal IVH are crucial in preventing further complications. Diagnostic procedures, such as cranial ultrasounds or magnetic resonance imaging, may be performed to assess the extent of bleeding and guide treatment decisions. Treatment options for IVH focus on supportive care, minimizing additional brain injury, and addressing associated complications like hydrocephalus.
Overall, recognizing the symptoms of neonatal intraventricular hemorrhage is vital for prompt diagnosis and intervention. Careful monitoring of at-risk infants, including premature babies, can help identify signs of IVH and facilitate appropriate medical interventions.
Common Risk Factors and Causes
Neonatal intraventricular hemorrhage (IVH) is a serious condition that occurs primarily in premature infants. It involves bleeding in the brain’s ventricular system, which can lead to long-term complications if not promptly recognized and treated. Understanding the common risk factors and causes associated with neonatal IVH is crucial for early detection and appropriate intervention. Here are some key factors to consider:
- Preterm Birth: Premature infants, born before 37 weeks of gestation, are at a significantly higher risk of developing IVH. The earlier the delivery, the greater the risk. Immature blood vessels in the brain are more susceptible to bleeding, making preterm babies more vulnerable.
- Low Birth Weight: Babies with low birth weight, especially those weighing less than 1,500 grams, are more prone to experiencing IVH. Inadequate nutrition and underdeveloped blood vessels can contribute to the fragility of brain tissues, increasing the risk of bleeding.
- Respiratory Distress Syndrome (RDS): The presence of RDS, a common condition in premature infants, heightens the likelihood of IVH. Insufficient lung development leads to low oxygen levels in the blood, impairing blood flow to the brain and increasing the likelihood of bleeding.
- Infection: Neonatal IVH risk is amplified by infections during pregnancy, delivery, or after birth. Infections such as maternal chorioamnionitis (inflammation of the fetal membranes) or neonatal sepsis can trigger an inflammatory response, potentially damaging fragile blood vessels in the brain.
- Intraventricular Catheterization: The use of intraventricular catheters in premature infants, often necessary for monitoring and treating other conditions, can inadvertently lead to IVH. The manipulation of delicate brain structures during catheter insertion or removal can cause bleeding.
It’s important for healthcare professionals to be vigilant in recognizing these risk factors and promptly identifying the symptoms of neonatal IVH. Early signs may include abnormal levels of consciousness, seizures, bulging fontanelles, and abnormal eye movements. Timely imaging studies, such as cranial ultrasound or magnetic resonance imaging (MRI), can help confirm the diagnosis and guide appropriate treatment.
By understanding the common risk factors and causes associated with neonatal IVH, healthcare providers can enhance their ability to identify at-risk infants and implement preventive measures. Furthermore, prompt intervention and specialized care can minimize the potential long-term impact of IVH, maximizing the chances of a favorable outcome for these vulnerable newborns.
Early Signs and Symptoms to Look Out For
Recognizing the symptoms of neonatal intraventricular hemorrhage (IVH) is crucial for prompt diagnosis and treatment. IVH refers to bleeding in the brain’s ventricles, most commonly affecting premature infants. While some cases may present with no obvious signs, there are several early symptoms to be aware of. Being vigilant and seeking medical attention if any of these signs are observed can significantly improve outcomes for affected infants.
- Abnormal muscle tone: Infants with IVH may exhibit either floppy (hypotonia) or rigid (hypertonia) muscle tone.
- Seizures: Seizure activity, including jerking movements or staring spells, can indicate the presence of IVH.
- Feeding difficulties: IVH can impact a baby’s ability to suck and swallow effectively, leading to difficulties in feeding or poor weight gain.
- Abnormal eye movement: Rapid, uncontrolled eye movements or the inability to focus on objects may be a sign of IVH.
- Discolored skin: In some cases, the baby’s skin may appear pale or bluish due to decreased oxygenation caused by IVH.
- Excessive crying: Infants with IVH may exhibit prolonged periods of intense crying without apparent cause.
- Bulging fontanelle: The soft spot on a baby’s head may appear tense or bulging when IVH is present.
- Altered level of consciousness: IVH can cause lethargy, irritability, or decreased responsiveness to stimuli.
If you notice any of these signs or symptoms, it is crucial to consult a healthcare professional immediately. Early detection and intervention can help prevent further complications associated with neonatal intraventricular hemorrhage, such as hydrocephalus or long-term neurological deficits. Always trust your instincts as a parent or caregiver and seek medical advice if you suspect something may be wrong with your newborn.
The Importance of Prompt Diagnosis and Treatment
Recognizing the Symptoms of Neonatal Intraventricular Hemorrhage is crucial for ensuring timely diagnosis and treatment. This condition, characterized by bleeding in the ventricles of a newborn’s brain, can have serious consequences if not addressed promptly. Here, we explore why prompt diagnosis and treatment are vital in managing neonatal intraventricular hemorrhage.
1. Prevention of complications: Timely identification allows healthcare professionals to intervene early, reducing the risk of complications and long-term damage. Addressing the underlying cause and implementing appropriate treatment strategies can help minimize the impact on the infant’s neurological development.
2. Improved prognosis: The earlier neonatal intraventricular hemorrhage is detected, the better the prognosis. Prompt treatment can prevent the condition from worsening and may increase the chance of a positive outcome. It allows for timely medical interventions, such as transfusions or surgical procedures, if necessary.
3. Preemptive management strategies: Early diagnosis enables healthcare providers to develop individualized management plans tailored to the specific needs of the infant. These plans may include close monitoring, specialized care in a neonatal intensive care unit, and the administration of medications or therapies to optimize recovery.
4. Prevention of further complications: Timely identification of neonatal intraventricular hemorrhage also allows for the prevention of secondary complications. Healthcare professionals can actively monitor and manage conditions such as hydrocephalus (abnormal accumulation of cerebrospinal fluid) or infection, which can arise as consequences of the initial hemorrhage.
5. Support for families: Prompt diagnosis helps alleviate anxiety and uncertainty for families who may be concerned about their newborn’s health. By promptly recognizing and explaining the condition, healthcare providers can provide reassurance, education, and the necessary support network to assist families through the treatment journey.
In conclusion, the prompt diagnosis and treatment of neonatal intraventricular hemorrhage are crucial for improved outcomes and minimizing long-term complications. Recognizing the symptoms early allows for timely intervention, personalized management plans, and the prevention of further issues. Through prompt action, healthcare professionals can provide the best possible care to support both the infant and their family.
Recognizing the Symptoms of Neonatal Intraventricular Hemorrhage
Neonatal intraventricular hemorrhage (IVH) refers to bleeding within the brain’s ventricular system in newborn babies. It is a serious condition that can lead to complications and long-term neurological issues if not recognized and treated promptly. Recognizing the symptoms of IVH is crucial for early intervention and better outcomes for affected infants.
Here are some key indicators to help recognize the symptoms of neonatal intraventricular hemorrhage:
1. Increased or abnormal head size: Infants with IVH may have an abnormally large or rapidly expanding head circumference due to the accumulation of blood in the ventricles of the brain. This swelling may be noticeable soon after birth or within the first few days.
2. Changes in muscle tone: IVH can disrupt the normal control of muscle movements. Infants may display floppy or hypotonic muscles (reduced muscle tone) or develop hypertonic muscles (increased muscle stiffness).
3. Behavioral changes: Watch out for changes in an infant’s behavior. They may become irritable, excessively sleepy, or experience sudden episodes of unexplained fussiness. These behavioral changes can be indicative of neurological distress caused by IVH.
4. Unexpected respiratory issues: Infants with IVH may exhibit difficulties in breathing, including irregular or rapid breathing patterns. They may also experience apnea (pauses in breathing) or require oxygen supplementation.
5. Seizures: Neonatal IVH can trigger seizures in affected infants. Seizures may manifest as repetitive twitching or jerking movements, staring spells, or unusual eye movements. Prompt medical attention is necessary if seizures occur.
6. Poor feeding and swallowing difficulties: Babies with IVH may find feeding challenging. They may have difficulty latching or sucking, leading to poor weight gain. Swallowing difficulties can result in choking or frequent regurgitation.
If you notice any of these symptoms, it is essential to seek immediate medical attention. Early diagnosis and intervention can help minimize the complications associated with neonatal intraventricular hemorrhage. Do not hesitate to consult a healthcare professional for a thorough evaluation and appropriate management.
Long-Term Effects and Complications
Neonatal Intraventricular Hemorrhage (IVH) is a serious condition that can have long-term effects and complications on the affected child’s health and development. Here, we will discuss some of these potential issues:
- Neurodevelopmental delays: Babies who experience IVH may be at an increased risk of developing neurodevelopmental delays. These delays can affect various aspects, including motor skills, cognition, learning abilities, and overall intellectual development.
- Cerebral palsy: Severe cases of IVH can lead to the development of cerebral palsy, a condition that affects muscle control and coordination. Children with cerebral palsy may have difficulties with movement, speech, and other physical activities.
- Intellectual disabilities: Depending on the severity of the IVH and its impact on the brain, children may experience intellectual disabilities. These disabilities can range from mild to severe and may affect the child’s ability to learn, communicate, and solve problems.
- Behavioral and emotional challenges: IVH can also contribute to behavioral and emotional challenges in affected children. They may exhibit issues such as impulsivity, hyperactivity, difficulty concentrating, and emotional regulation problems.
- Vision and hearing impairments: In some cases, IVH can result in visual or hearing impairments. Visual impairments may include partial or complete blindness, while hearing impairments can range from mild to severe hearing loss.
- Epilepsy: Children who have experienced IVH may have an increased risk of developing epilepsy, a neurological disorder characterized by recurrent seizures. The severity and frequency of seizures can vary from person to person.
It is important to note that not all infants who experience IVH will develop long-term complications. The extent of the complications depends on factors such as the severity of the bleeding, the affected brain areas, and the overall health and development of the child. Early intervention, appropriate medical care, and rehabilitative therapies can significantly improve outcomes and minimize the potential long-term effects of IVH.