Varicose Veins: Prevention and Treatment Options
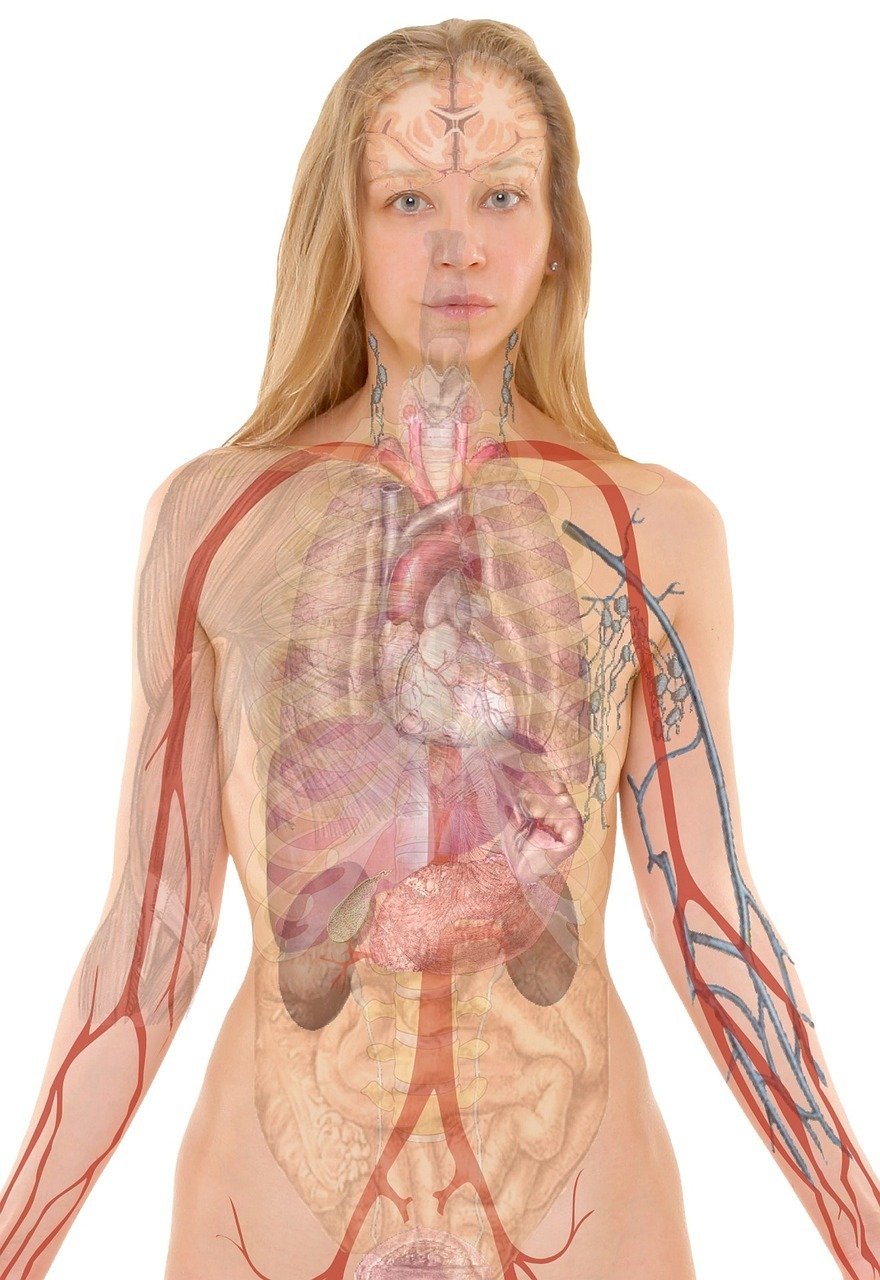
Table of Contents
Understanding Varicose Veins: Causes and Risk Factors
Varicose veins are a common condition that affects millions of people worldwide. They are enlarged, twisted veins that usually appear on the legs and can cause discomfort and pain. Understanding the causes and risk factors of varicose veins is essential for prevention and effective treatment.
Here are some common causes and risk factors associated with varicose veins:
- Age: As we age, the valves in our veins may weaken, leading to the development of varicose veins.
- Gender: Women are more prone to developing varicose veins compared to men. Hormonal changes during pregnancy and menopause can contribute to their development.
- Family history: If your parents or close family members have varicose veins, you have a higher risk of developing them.
- Obesity: Excess weight puts additional pressure on the veins, making them more prone to becoming varicose.
- Prolonged standing or sitting: Jobs that require long periods of standing or sitting can increase the risk of varicose veins.
- Poor circulation: Conditions like deep vein thrombosis or chronic venous insufficiency can impair proper blood flow, leading to varicose veins.
- Inactivity: Lack of exercise and a sedentary lifestyle can weaken the veins and increase the likelihood of developing varicose veins.
While some risk factors like age and family history cannot be changed, there are preventive measures and treatment options available to manage varicose veins:
- Regular exercise: Engaging in physical activity, particularly exercises that promote leg strength and circulation, can help prevent varicose veins.
- Maintain a healthy weight: By maintaining a healthy weight, you can reduce the pressure on your veins and lower the risk of varicose veins.
- Elevate your legs: Elevating your legs above the heart level can help improve blood flow and alleviate symptoms of varicose veins.
- Avoid prolonged sitting or standing: Take breaks and move around if your job requires long periods of sitting or standing.
- Compression stockings: These specially designed stockings apply pressure to the legs, helping to improve blood flow and reduce the appearance of varicose veins.
- Sclerotherapy or laser treatment: These minimally invasive procedures can be used to treat varicose veins by closing off the affected veins and redirecting blood flow.
It is important to consult with a healthcare professional for an accurate diagnosis and personalized treatment plan if you suspect you have or are at risk of developing varicose veins. They can provide guidance on the most suitable preventive measures and treatment options based on your individual circumstances.
Lifestyle Changes for Varicose Vein Prevention
Varicose veins are a common condition that affects many individuals. While there are various treatment options available, prevention is always better than cure. Making certain lifestyle changes can significantly reduce your risk of developing varicose veins or prevent existing ones from worsening. Here are some changes you can incorporate into your daily routine:
- Exercise regularly: Engage in activities that promote good blood circulation, such as walking, swimming, or cycling. Regular exercise helps to strengthen the leg muscles and improve blood flow.
- Maintain a healthy weight: Excess weight puts additional pressure on the veins in your legs, increasing the likelihood of varicose veins. By maintaining a healthy weight, you can reduce this pressure and prevent the formation of varicose veins.
- Elevate your legs: Whenever possible, elevate your legs above heart level to help improve blood circulation. This can be done by propping your legs up on a pillow or using a leg rest while sitting.
- Avoid prolonged sitting or standing: Sitting or standing for long periods can lead to poor blood circulation. If your job requires long periods of sitting or standing, make sure to take breaks and move around every hour.
- Wear compression stockings: Compression stockings can help improve blood flow in your legs by applying pressure to the veins. They are especially beneficial when traveling or during long periods of inactivity.
- Follow a healthy diet: Incorporate foods rich in fiber, such as fruits, vegetables, and whole grains, into your diet. A high-fiber diet helps prevent constipation, which can contribute to the development of varicose veins.
- Avoid tight clothing: Tight clothing, especially around the waist, groin, and legs, can restrict blood flow and contribute to the formation of varicose veins. Opt for loose-fitting clothes instead.
- Quit smoking: Smoking can weaken the walls of your blood vessels, making them more susceptible to damage and increasing the risk of varicose veins. Quitting smoking not only benefits your overall health but also reduces your chances of developing varicose veins.
By implementing these lifestyle changes, you can reduce your risk of varicose veins and promote overall leg health. However, if you already have varicose veins or experience discomfort, it is essential to consult with a healthcare professional for diagnosis and appropriate treatment options.
Natural Remedies for Varicose Veins
Varicose veins are a common condition that affects many individuals. They are enlarged, twisted veins that usually appear on the legs and can cause discomfort, pain, and swelling. While there are medical treatments available for varicose veins, there are also several natural remedies that can help prevent and alleviate symptoms. Here are some natural remedies that you can try:
- Exercise regularly: Engaging in physical activity can improve blood circulation and help prevent varicose veins. Activities such as walking, swimming, and cycling are particularly beneficial.
- Elevate your legs: Raising your legs above the heart level can reduce swelling and promote better blood flow. Whenever possible, prop your legs up on a pillow or elevate them using a footrest.
- Wear compression stockings: Compression stockings provide pressure to the veins, helping to improve blood flow and reduce the risk of varicose veins. They are available in different compression levels and can be worn throughout the day.
- Follow a healthy diet: Incorporate foods that promote healthy circulation, such as high-fiber foods, fruits, vegetables, and foods rich in antioxidants. Avoid excessive salt intake, as it can contribute to water retention and swelling.
- Avoid prolonged sitting or standing: Sitting or standing for long periods can put extra pressure on the veins. Take breaks and move around regularly to prevent blood from pooling in the legs.
- Practice weight management: Maintaining a healthy weight can reduce the strain on your veins and minimize the risk of developing varicose veins.
- Use herbal remedies: Certain herbs like horse chestnut, butcher’s broom, and gotu kola have been traditionally used to improve blood circulation and strengthen vein walls. However, it is important to consult with a healthcare professional before trying any herbal supplements.
- Avoid tight clothing: Wearing tight clothes, especially around the waist, groin, and legs, can restrict blood flow and contribute to the development of varicose veins. Opt for loose-fitting clothing instead.
While these natural remedies can be effective in preventing and managing varicose veins, it is essential to consult with a healthcare professional for a proper diagnosis and advice on the best course of treatment for your specific condition.
Medical Treatments for Varicose Veins
Varicose veins are a common condition that can cause discomfort and cosmetic concerns. While prevention is key, sometimes medical treatments are necessary to alleviate symptoms and improve the appearance of these veins. Here are some medical treatment options for varicose veins:
- Sclerotherapy: This is a popular treatment for small to medium-sized varicose veins. A solution is injected into the affected veins, causing them to collapse and fade over time. Multiple sessions may be required to achieve desired results.
- Endovenous Laser Ablation (EVLA): This minimally invasive procedure involves inserting a laser fiber into the affected vein, which emits laser energy to heat and close the vein. EVLA is effective for larger varicose veins and usually requires local anesthesia.
- Radiofrequency Ablation (RFA): Similar to EVLA, RFA uses radiofrequency energy to heat and close off the affected vein. This procedure is also minimally invasive and provides long-lasting results.
- Phlebectomy: This procedure involves making small incisions to remove sections of the affected vein. Phlebectomy is typically performed under local anesthesia and is suitable for larger varicose veins.
- Endovenous Chemical Ablation: In this procedure, a special chemical is injected into the affected vein, causing it to close and eventually disappear. Endovenous chemical ablation is effective for larger varicose veins and may require compression stockings post-treatment.
It’s important to consult with a healthcare professional, such as a vascular specialist or phlebologist, to determine the most suitable treatment option based on your specific condition and medical history. They will assess the severity of your varicose veins and recommend the most appropriate treatment plan.
While medical treatments can provide relief and improve the appearance of varicose veins, it’s essential to adopt preventive measures to minimize the risk of developing new ones or worsening existing ones. Regular exercise, maintaining a healthy weight, elevating legs when resting, avoiding prolonged periods of standing or sitting, and wearing compression stockings are some preventive strategies to consider.
Remember, early intervention and proper medical care can help manage varicose veins effectively and enhance your overall well-being.
Surgical Interventions for Varicose Veins
While conservative measures can help manage varicose veins, surgical interventions may be necessary for more severe cases. Here are some surgical treatment options:
- Vein Ligation and Stripping: This procedure involves tying off and removing the affected veins. It is typically done under general anesthesia and may require a hospital stay. Vein ligation and stripping are effective in treating large varicose veins.
- Endovenous Laser Ablation: Also known as EVLA or EVLT, this minimally invasive procedure involves inserting a thin laser fiber into the affected vein. The laser generates heat, causing the vein to close off and eventually disappear. EVLA is effective for treating both small and large varicose veins.
- Sclerotherapy: This procedure involves injecting a solution directly into the varicose veins, causing them to collapse and fade away over time. Sclerotherapy is often used for smaller varicose veins and spider veins. It can be performed in a doctor’s office and typically requires multiple sessions for optimal results.
- Phlebectomy: This surgical procedure involves removing varicose veins through small incisions made in the skin. Phlebectomy is typically performed under local anesthesia and does not require stitches. It is effective for treating surface varicose veins and is often combined with other treatments for comprehensive results.
- Endoscopic Vein Surgery: This procedure is usually reserved for severe cases of varicose veins. It involves using a small camera (endoscope) to visualize and remove the affected veins. Endoscopic vein surgery is performed under general anesthesia and may require a longer recovery period.
It is important to consult with a qualified healthcare professional to determine the most appropriate surgical intervention for your varicose veins. They will consider your individual case, medical history, and preferences to develop a personalized treatment plan.